Derek Welsbie, MD, PhD: Glaucoma is now the number one reason people go irreversibly blind, and sadly, it’s getting worse.
Milica Margeta, MD, PhD: Neurodegeneration means loss of neurons. They’re basically the little individual units that come together and give us the ability to think, feel, see, hear, etc. What my team is trying to understand is really, why do neurons die in glaucoma? Why do we get loss of vision to begin with? And then by understanding these mechanisms and also how they’re similar to brain diseases, we hope to develop new treatments that will start this process.
Anna La Torre, PhD: We benefit from the work that’s been done previously by the Catalyst for a Cure 1 [the Inaugural Initiative], and Catalyst for a Cure 2 [the Biomarker Initiative] groups, because they set up the foundation that allows us to understand: what is glaucoma?
Derek Welsbie: Really, one of the main accomplishments of this research has been to turn glaucoma from a pressure disease to neurodegenerative disease.
Milica Margeta: Current treatments for glaucoma all focus on lowering the eye pressure, which is one of the main risk factors. Having said that, many patients proceed to lose vision and go blind despite everything we can do for their pressure control.
Derek Welsbie: The way that the CFC research will impact patients really comes in two flavors. The first is a short-term goal for the Catalyst for a Cure, which is coming up with neuroprotective therapies that preserve vision. That’s something that could happen over the course of the next one, two, three, five years, something in that timeframe. The other goal for our research is to restore vision, and that’s something that’s a little bit more of a long-term goal because it’s a harder challenge.
Sandro Da Mesquita, PhD: As part of this consortium of Catalyst for a Cure, we are looking to bring people with different expertise together to try to understand: what are common features of different neurogenerative disorders?
Milica Margeta: Glaucoma Research Foundation is currently funding two separate consortiums.
Anna La Torre: The advantage of having two teams working side by side is that we can work on the project that we have already set, and at the same time, we can take advantage of the other team and really establish bridges between these two lines of research.
Derek Welsbie: So, if you look at my lab, I’m a glaucoma clinician/scientist. I do glaucoma research, but then you look at Anna La Torre, who’s a developmental biologist or Xin Duan, who does retinal ganglion cell physiology.
Milica Margeta: One of us is an immunologist who heavily studies Alzheimer’s disease. Another team member is a cancer specialist. We have a bioinformatician, which basically will enable us to look at these disease processes in much finer detail than has ever been done before.
Derek Welsbie: And these wouldn’t necessarily be the first people you would think of as studying glaucoma. However, when you bring their expertise together, you form a team that allows us to study stem cells and use them for retinal transplantation, or understanding which are the most resistant subtypes of retinal ganglion cells that we can leverage for a neuroprotective strategy in glaucoma.
Sandro Da Mesquita: We believe that by doing so, we’ll be able to push science forward in this field and really improve patient’s quality of life in the near future.
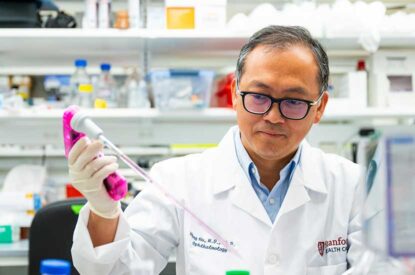
Derek Welsbie: In the last three years, we’ve built these tools to identify which types of optic nerve cells are most resistant to glaucoma. We’ve been able to identify those genes that seem to control optic nerve cell death and regeneration. Now, the challenge for the next three years is to put that together as a therapy.
Anna La Torre: I’m very excited to have the opportunity to try all these experiments and try to transplant new cells and develop technologies to facilitate ways for the cells to survive better and grow cables to connect better with both the retina and the brain.
Sandro Da Mesquita: It’s truly because of the power of philanthropy and of donors that we are able to do this groundbreaking research without being constantly worried about funding issues or other type of distractions that drive us away from what really matters, which is to focus on research, focus on pathological mechanisms of disease that we should try to better understand.
Derek Welsbie: Having multi-year funding and a long-term commitment from the GRF is really critical. If you only have one year funding, then you need to produce your results and tidy everything up by the end of one year. So you have to ask a relatively small question. In contrast, if you have multi-year funding, you can ask bigger questions. You can swing for the fences. Not only are we looking to develop therapies for glaucoma, but because glaucoma is a neurodegenerative process, the things that we develop, the things that we understand have impact on all these other horrible neurodegenerative diseases out there like Alzheimer’s, Parkinson’s, ALS.
Sandro Da Mesquita: We are studying and focusing most often in very particular aspects of biology molecules, biochemical processes, but in order to fully understand these, to be able to treat it, we have to go to these very, very fundamental scientific principles. And we can only do that through your support, which is really, really important. And I’m sure that altogether as a team, scientists and supporters from GRF, we will find better therapies for patients.
Milica Margeta: What I think is really remarkable about this consortium is that essentially we were put together and given this very open-ended set of approaches in a very open-ended way. And I think that is really exciting and has a tremendous amount of potential to generate new insights and completely novel hypotheses, completely novel ways of looking at neurodegeneration that people haven’t thought of before.
End transcript.