Testing for Glaucoma
Glaucoma is an eye disease that usually has no symptoms in its early stages
Without proper treatment, glaucoma can lead to blindness. The good news is that with regular eye exams, early detection, and treatment, you can preserve your sight.

To accurately and safely diagnose glaucoma, your eye doctor will check five factors during your glaucoma eye test:
- Tonometry (eye pressure test): A measure of the pressure inside the eye (intraocular pressure or IOP)
- Ophthalmoscopy (examination of the back of the eye): Examination of the shape and color of the optic nerve, also called a dilated eye exam
- Perimetry (visual field test): A test that measures your field of vision
- Gonioscopy (examination of the eye’s drainage angle): Examination of the angle in the eye where the iris meets the cornea
- Pachymetry (measures the thickness of the cornea): A measure of the thickness of the cornea
Video: Glaucoma Eye Exams
Watch this video to see what’s involved in a glaucoma eye exam.
What to Expect During Glaucoma Tests
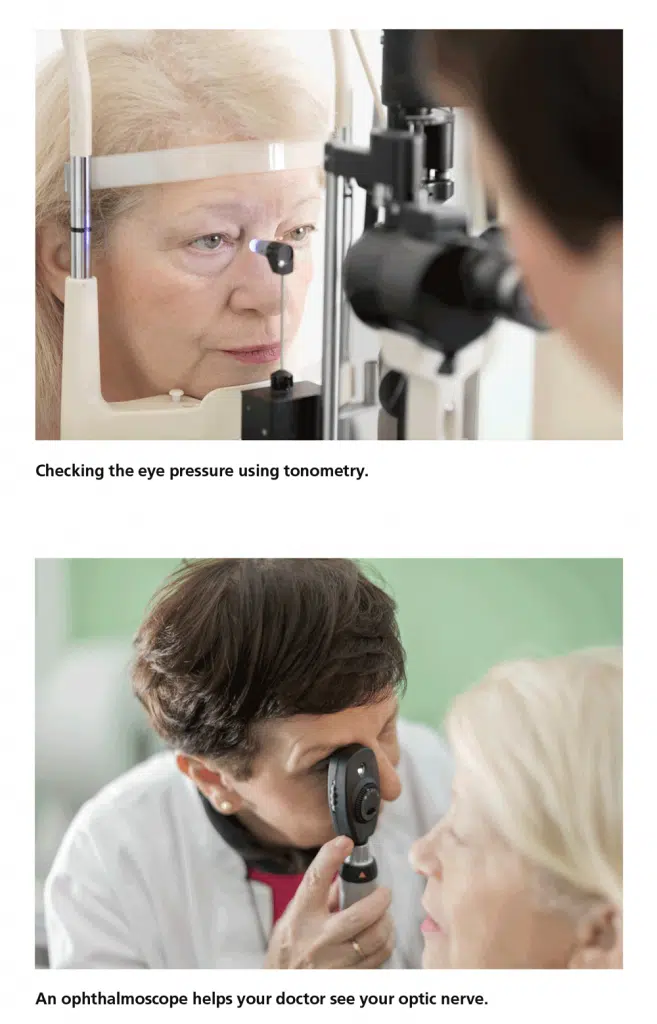
Tonometry (Eye Pressure Test)
During tonometry, also known as an eye pressure test) eye drops are used to numb the eye. Then a doctor or technician uses a device called a tonometer to measure the eye pressure. A small amount of pressure is applied to the eye by a small device. The average range for eye pressure is 10–21 mm Hg (“mm Hg” refers to millimeters of mercury, a scale used to record eye pressure.) The level of eye pressure at which glaucoma develops is not the same for everyone, and some people can get glaucoma even if their eye pressures are within the average range of 10–21 mm Hg.
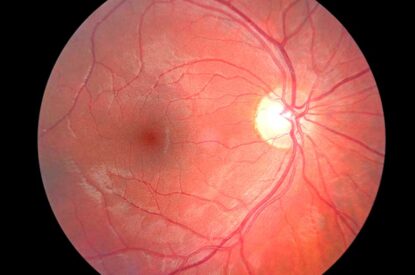
Ophthalmoscopy (Examination of the Back of the Eye)
Eye drops are used to dilate the pupil so that the doctor can see into your eye with a special lens to examine the shape and color of the optic nerve and note whether there is glaucoma damage. You may need to wait in a waiting room for your eyes to fully dilate. The doctor will use a small device to shine light on and magnify the optic nerve. The doctor will check if the optic nerve is cupped or not a healthy pink color, which may be a cause for concern.
Various laser-based imaging technologies can also be used to examine the optic nerve and of these, Optical Coherence Tomography (OCT) is the most commonly used. OCT measures the reflection of laser light (much like ultrasound measures the reflection of sound) and can directly measure the thickness of the nerve fiber layer. Imaging your optic disc over time during multiple visits can help detect progressive loss of optic nerve fibers.
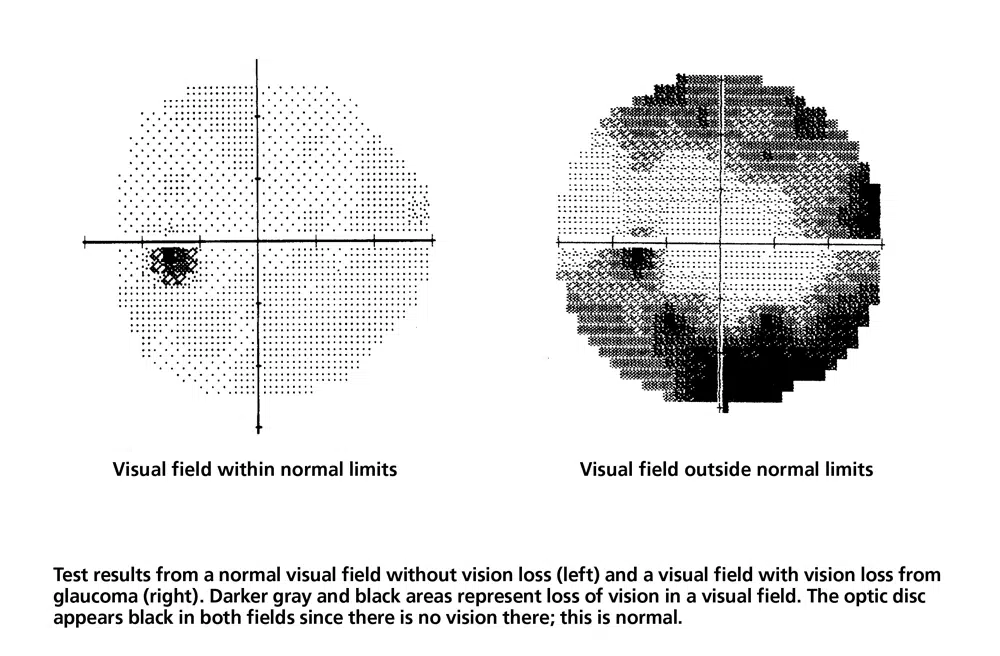
Perimetry (Visual Field Test)
Perimetry (or “visual field testing”) produces a map of your field of vision. This test will help your doctor determine whether your vision has been affected by glaucoma.
During this test, you will be asked to look straight ahead and then press a button whenever you see a spot of light in your peripheral (side) vision. The spots of light will vary in intensity such that some are very easy to see and others are not visible even when vision is normal. Try to relax, blink normally, and respond as accurately as possible during the test. Don’t worry if you feel you missed a spot as areas are automatically retested. Your test performance may vary if you are tested at the end of a long day.
Your doctor may want you to repeat the test to see if the results are the same. After glaucoma has been diagnosed, visual field tests are usually done one to two times a year to check for any changes in your vision.
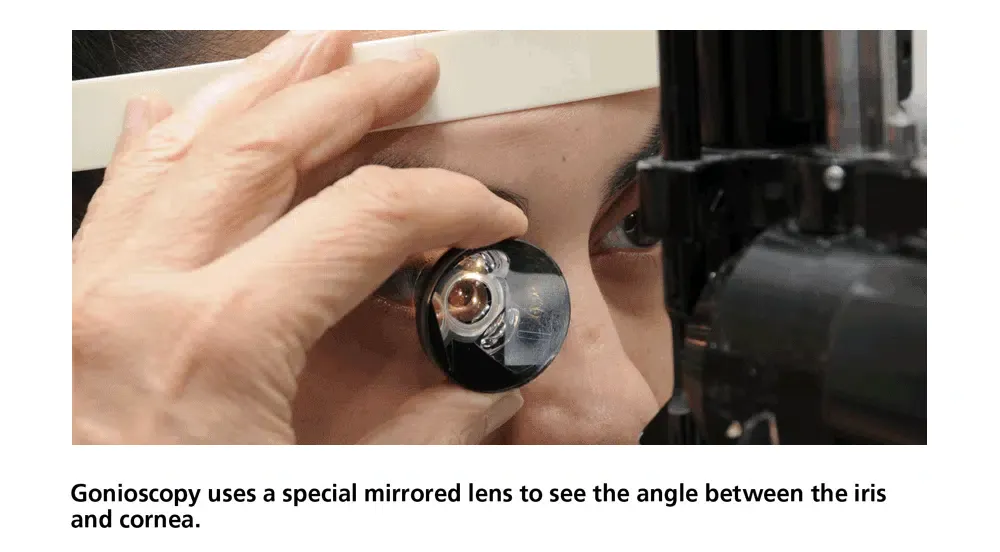
Gonioscopy (Examination of the Eye’s Drainage Angle)
Gonioscopy is a diagnostic exam that helps determine whether the angle where the iris meets the cornea is open or closed. During the exam, eye drops are used to numb the eye, and a special hand-held lens is gently placed on the eye for a few moments. This special lens includes a mirror that allows the doctor to see the angle between the iris and cornea to determine its status.
Pachymetry (Measures the Thickness of the Cornea)
Pachymetry is a simple, painless test that measures the thickness of the cornea—the clear window at the front of the eye—using a probe that is gently placed on your eye. A thin cornea is a risk factor for glaucoma. Corneal thickness also has the potential to influence eye pressure readings. For example, if a cornea is thicker than average, pressure readings with a tonometer may be higher than the actual pressure and if a cornea is thinner pressure readings may be lower than actual. Using pachymetry, your doctor can better understand your eye pressure readings and develop a treatment plan that is right for you.
Learn More