Saving Sight in Glaucoma: Why the Brain May Hold the Key
What causes vision loss in glaucoma? First is elevated ocular pressure, and second is damage to the optic nerve, which is the structure that sends visual information to the brain.
What causes vision loss in glaucoma?
There are two common answers that at first may seem disparate: the first is pressure, as in elevated ocular pressure, and the second is damage to the optic nerve, which is the structure that sends visual information to the brain. Both answers are correct.
Glaucoma involves sensitivity to ocular pressure (not just elevated pressure) that is translated or transduced to stress that degrades the optic nerve over time. Current glaucoma therapies lower pressure using eye drops, surgery, or both in order to reduce stress transduced to the optic nerve. This approach is effective for many patients. But for those who continue to lose vision, where should we turn for new clinical therapies?
One idea is to consider where ocular pressure exerts its influence: the optic nerve head. This structure in the back of the eye defines where nerve fibers leave the retina and enter the optic nerve. The nerve head contains lateral structures that support these fibers but also couple the nerve to the rest of the eye. In this way, pressure in the front of the eye can cause stress to the optic nerve. While we do not understand precisely how this stress is conveyed, we do know that aging of the nerve head is likely to contribute to its susceptibility. By addressing age-related factors, new research might reveal therapies based on reducing the sensitivity of the nerve head to pressure.
What about the optic nerve itself? Like the brain, the optic nerve and retina are part of the central nervous system. Once damaged beyond a certain point, these structures cannot heal. For patients who have lost substantial optic nerve tissue in glaucoma, the hope of regenerative medicine is to restore connectivity with the brain by introducing new nerve fibers or inducing damaged ones to regrow.
Another area of promise that may be forthcoming leverages the idea that increasing brain activity in some cases increases its resistance to stress. Catalyst for a Cure (CFC) research has demonstrated a “window of structural persistence” in which connectivity between the optic nerve and brain remains even when glaucoma affects visual function. During this “window,” optic nerve fibers attempt to boost their electrical activity through natural self-repair mechanisms.
Research by CFC investigators shows that enhanced activity can also help optic nerve fibers regenerate. Perhaps the best approach to a new type of nerve-based glaucoma treatment would combine optic nerve regenerative techniques with those that promote intrinsic repair in the brain.
Article by David J. Calkins, PhD. First published September 13, 2016; Last reviewed on May 11, 2022.
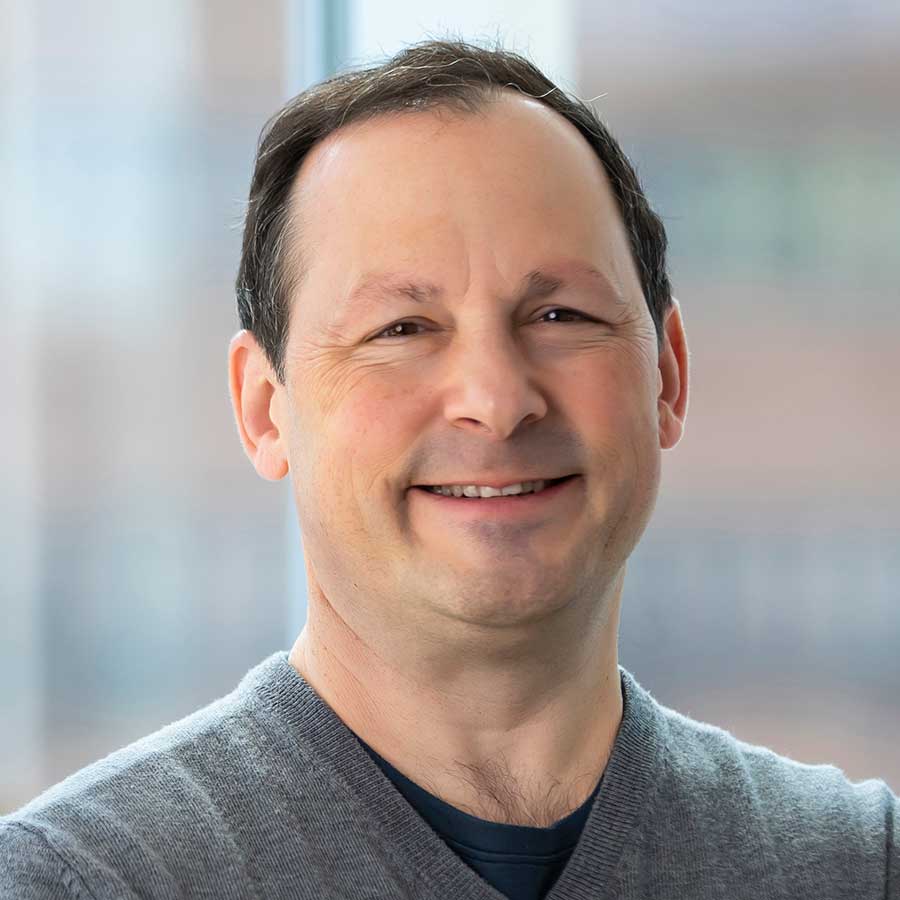
David J. Calkins, PhD
Dr. Calkins is the Denis M. O’Day Professor of Ophthalmology and Visual Sciences and Vice-Chairman and Director for Research at The Vanderbilt Eye Institute, Vanderbilt University Medical Center in Nashville, Tennessee.