Traumatic Glaucoma
What is Traumatic glaucoma?
Traumatic glaucoma is any glaucoma caused by an injury to the eye. This type of glaucoma can occur both immediately after an injury to the eye or years later.
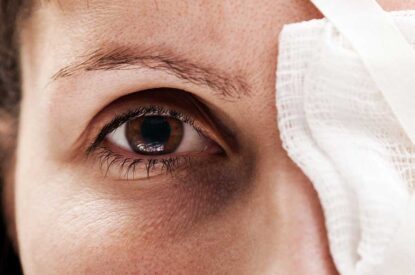
It can be caused by injuries that “bruise” the eye (called blunt trauma) and injuries that penetrate the eye.
Conditions such as severe nearsightedness, previous injury, infection or prior surgery may also make the eye more vulnerable to a serious eye injury.
Blunt Trauma
As a result of an immediate injury, traumatic glaucoma is most commonly caused by blunt trauma, which is an injury that doesn’t penetrate the eye, such as a blow to the head or an injury directly on the eye.
The most common cause is from sports-related injuries, such as baseball or boxing. Normally, the eye fluid flows out of the front part of the eye through the pupil and then is absorbed into the bloodstream through a meshwork of drainage canals around the outer edge of the iris.
When a blunt trauma occurs, damage to this system can occur. The most common cause is the ciliary body, the part of the eye that produces eye fluid, inside the eye tearing. This can cause bleeding inside the eye.
The excess amount of blood, plasma and debris can accumulate and clog the drainage system. This can lead to an increase in eye pressure, which can damage the optic nerve.
Elevated eye pressure due to blunt trauma is treated by keeping the eye pressure at safe levels while the eye drains the excess blood out. Glaucoma medications to control the eye pressure are usually tried first. If this is not sufficient to control the eye pressure, surgery may be necessary.
The elevated eye pressure following blunt trauma is temporary in most cases. It is important, however, to make sure to get regular follow-up eye exams.
In some cases, the damaged drainage canals in the eye can build up excess scarring. This scarring blocks fluid flow and can lead to glaucoma. This type of glaucoma, called angle recession glaucoma, can occur many years after the initial injury.
The angle recession is seen on an exam as a tear at the base of the iris where the drainage canals are. Angle recession glaucoma can be difficult to treat. Treatments can include medications that reduce fluid production in the eye, laser surgery or filtering surgery.
Penetrating Eye Injury
Traumatic glaucoma can also be caused by penetrating injuries to the eye, such as those caused by a sharp instrument or flying debris. The eye pressure is usually lower right after the injury occurs. Once the wound is closed, tissue inside the eye can become swollen and irritated, and bleeding can occur, causing the eye pressure to rise.
Short term rises in eye pressure are controlled in ways similar to cases of blunt trauma. However, damaged tissue and scarring from a penetrating eye injury can lead to blocked drainage canals.
Glaucoma due to a penetrating eye injury is best treated by preventive measures when the initial wound occurs. Corticosteroid therapy to help prevent tissue damage and scarring and antibiotics are an important component of initial treatment. Initial treatment can also include surgery to remove excess eye fluid or reduce swollen tissue.
If glaucoma does develop over the long term, medications that reduce the production of eye fluid are usually the first method of treatment, followed by filtering surgery.
Article by Ruth D. Williams, MD. Last reviewed on January 1, 2022.
Learn More