Pigmentary Glaucoma
What are Pigment Dispersion Syndrome and Pigmentary Glaucoma?
Pigment dispersion syndrome is a condition where pigment from the back of the iris (the colored part of the eye) is released and becomes trapped in the drainage system of the eye. The pigment could block the drain which could, in turn, lead to an increase in eye pressure.
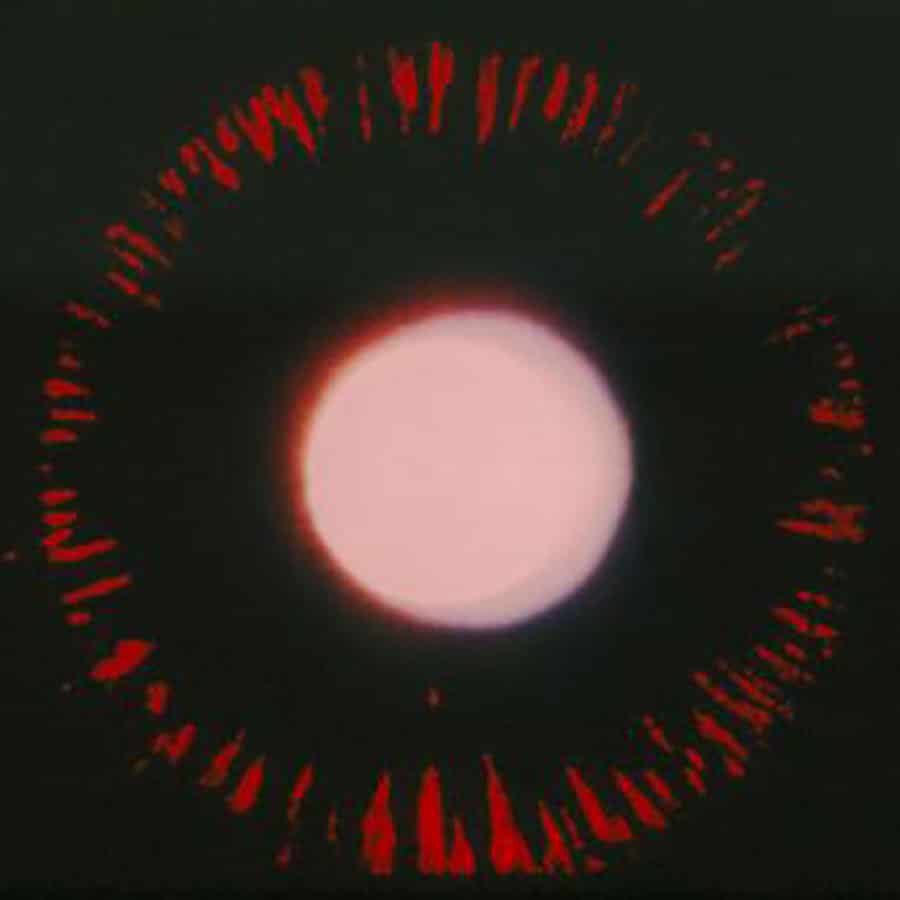
The features of pigment dispersion syndrome, such as excessive pigment in the drain and areas of pigment loss from the iris, can be detected during an eye examination.
Pigment dispersion syndrome is more common in young, Caucasian, male patients who are near-sighted. The eye pressure can significantly increase during exercise, but usually returns to normal.
These eye pressure spikes may cause symptoms such as blurry vision and rainbow colored haloes around lights. As patients age, there is less pigment dispersion, but the patient can still be at risk for developing glaucoma.
Video: Pigment Dispersion Syndrome And Pigmentary Glaucoma
This short video gives an overview of pigment dispersion syndrome and pigmentary glaucoma.
How Does Pigment Dispersion Syndrome Cause Glaucoma?
Pigment dispersion syndrome can lead to permanent damage to the drain and elevated eye pressure. Over time, the elevated eye pressure can damage the optic nerve, causing pigmentary glaucoma. Untreated glaucoma can lead to vision loss and eventually blindness.
How Can Doctors Treat Pigmentary Glaucoma?
The treatment of pigmentary glaucoma involves lowering the eye pressure using medications, lasers, or surgery. Unfortunately, it is difficult to reduce or eliminate the release of iris pigment. Therefore, attention is focused on reducing eye pressure.
Eye pressure-lowering medications cause either a decrease in fluid into the eye or an increase of fluid out of the eye. Depending on the severity of the disease, surgery can range from laser treatment as an outpatient to incisional surgery in the operating room.
The Takeaway
Pigment dispersion syndrome is a risk factor for developing glaucoma and patients who have this condition should be monitored regularly. Patients with pigmentary glaucoma can be treated successfully. Thankfully, with modern treatments, many patients are able to maintain excellent vision.
Article by Ninita Helen Brown, MD, PhD. First posted on January 1, 2017. Last reviewed on February 4, 2022.
Learn More



