How Glaucoma Progresses and What You Can Do to Protect Your Vision
Learn about the stages of glaucoma and how to protect your vision.
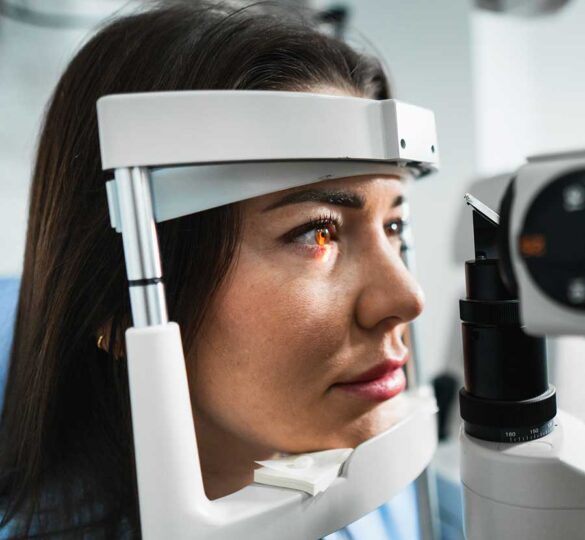
Glaucoma is a group of eye diseases that damage the optic nerve — often without early symptoms — and can lead to permanent vision loss if not treated. The good news: With timely diagnosis and the right treatment plan, most people can slow or stop vision loss.
Globally, glaucoma is a leading cause of irreversible blindness, affecting an estimated 80 million people worldwide as of 2020. In the US alone, more than 4 million people had glaucoma in 2022, yet up to half of those may be unaware they have it.
Although you can’t reverse vision loss from glaucoma, learning how the disease progresses helps you take the first crucial steps toward managing it effectively and preserving your sight.
The 4 Stages of Glaucoma Progression
The progression of glaucoma can generally be broken down into four practical stages.
1. Stage 1: Early/Pre-Glaucoma
- What It Means: Your doctor or medical records at this stage may use the term glaucoma suspect. That means you’re being evaluated for the possibility of glaucoma due to high-risk features, such as a family history of glaucoma, high eye pressure, or enlargement of the indentation in the optic nerve (cupping). At this stage, there are no noticeable symptoms, and your visual field tests are still normal.
- How It Affects Treatment: According to the Mayo Clinic, treatment may involve a watchful waiting approach or a regimen of laser therapy or prescription eye drops to lower intraocular pressure (IOP) and prevent damage. For those with high eye pressure (ocular hypertension) but no definitive nerve damage, treatment can significantly reduce the risk of developing glaucoma.
- Why Early Detection Matters: Catching glaucoma — or even its warning signs — early gives you the best chance to protect your sight.
2. Stage 2: Mild Glaucoma
- What It Means: Subtle, measurable damage to the optic nerve is now evident, but your peripheral vision test remains normal.
- How It Affects Treatment: Laser therapy (called selective laser trabeculoplasty [SLT]) or prescription eye drops are initiated or intensified to lower IOP. The goal is to halt the progression of nerve damage. At this stage, your doctor can set a target IOP and create a personalized plan to keep your vision healthy before any lasting damage occurs.
- Why Early Detection Matters: The earlier you begin consistent treatment, the better the long-term prognosis. Treatment at this stage is highly effective at preventing progression to more damaging stages.
3. Stage 3: Moderate Glaucoma
- What It Means: At this stage, damage to the optic nerve is more pronounced, and areas of peripheral vision loss are detectable. Critically, these small blind spots are usually unnoticed by the patient because their central vision remains unaffected, and the brain can compensate.
- How It Affects Treatment: Managing moderate glaucoma usually requires a more aggressive approach. Doctors may prescribe a combination of eye drops to reduce intraocular pressure (IOP) further, repeat laser treatments to improve fluid outflow, or recommend surgical procedures if pressure remains uncontrolled. The treatment goal is to preserve remaining vision and prevent further nerve damage.
- Why It Matters: At the moderate stage, patient experiences are diverse. Many patients remain truly asymptomatic. Other patients note that activities such as driving, reading, performing tasks in dim light, or navigating unfamiliar spaces can become challenging. Strict adherence to treatment and regular follow-up visits are crucial to protecting your vision and maintaining independence.
4. Stage 4: Severe Glaucoma
- What It Means: At this stage, glaucoma causes the most severe vision loss. Peripheral vision is damaged, and your central vision may be affected as well. Daily activities such as reading, navigating curbs and sidewalk cracks, and recognizing faces become more difficult. Consistent treatment and monitoring are essential to preserve remaining sight.
- How It Affects Treatment: The highest level of treatment is typically needed, often involving advanced surgical procedures (such as trabeculectomy or glaucoma drainage implant surgery) to drastically lower and maintain the lowest possible IOP. Low-vision aids and rehabilitation are sometimes necessary to help patients adapt to their remaining vision.
- Why Early Detection Matters: At this stage, your care team focuses on protecting the central vision you still have and helping you make the most of your remaining sight.
Protecting Your Vision
Protecting your vision starts with proactive care. Although glaucoma has no cure, you can make a powerful difference by detecting it early and managing it consistently. By taking these key steps, you can help preserve your sight and reduce your risk of vision loss.
- Get Regular Comprehensive Eye Exams: The American Academy of Ophthalmology generally recommends a comprehensive eye exam every two to four years if you are 40-54 and every one to three years if you are 55-64. If you have risk factors such as a family history of glaucoma, diabetes, or are over 60, your doctor will recommend more frequent screenings.
- Know Your Risk Factors: Glaucoma disproportionately affects African Americans and Hispanics, and risk increases significantly with age and family history.
- Follow Your Treatment Plan: If your doctor diagnoses glaucoma, you can protect your vision by using the prescribed therapies and keeping all follow-up appointments exactly as directed to maintain your target eye pressure.
Help Us Find a Cure
Don’t let the silent thief win. Schedule a comprehensive, dilated eye exam today.
While there’s no cure for glaucoma, advancements in research continue to bring us closer to finding one and restoring vision loss. You can help find a cure by donating cash, stock, or a vehicle. Your support will give hope to those living with glaucoma and accelerate our search for a cure and vision restoration.
The tireless work of researchers continues to enhance our understanding of glaucoma daily. As a result, there’s great hope for new and improved treatments, including innovative drug-delivery methods, laser treatments, and less-invasive surgical techniques. You can help make that happen!
Posted on December 23, 2025. Reviewed for medical accuracy by Sarah H. Van Tassel, MD.

Sarah Van Tassel, MD
Sarah H. Van Tassel, MD is a fellowship-trained glaucoma specialist and Director of the Glaucoma Service and Glaucoma Fellowship at Weill Cornell Medicine Ophthalmology in New York City.