2023 Research Update from the Catalyst for a Cure Vision Restoration Team
The Catalyst for a Cure Vision Restoration Initiative (CFC3) is seeking innovative ways to regrow or replace retinal ganglion cells and axons, which make up the optic nerve.
The Catalyst for a Cure Vision Restoration initiative has three major goals:
- Developing neuroprotective therapies to halt the progression of vision loss from glaucoma;
- Developing strategies for visual restoration using cell transplantation to replace lost optic nerve cells;
- Reconnect the eye to the brain to restore visual functions to improve the function of injured optic nerve cells.
In the past year, the Catalyst for a Cure Vision Restoration Team has made significant progress on multiple fronts.
First, we have advanced the field of neuroprotection:
In order to identify novel neuroprotective targets for glaucoma, the team measured the change in the expression of every gene in the genome. For genes that change, there are two possibilities: genes that change their expression as a consequence of the injury or genes that change because they are the cause. In the former, one would expect glaucoma to continue, even in the absence of that gene, while in the latter, there should be less glaucoma if that gene is removed. To distinguish between these two possibilities, the collaboration uses molecular scissors called CRISPR to delete candidate genes and test their role in a mouse model of glaucoma developed by one of the investigators.
Second, we have made the following progress with the cell replacement:
In the past, we identified that a major obstacle to these technologies was the poor survival of the cells generated in Petri dishes after transplant attempts. Unfortunately, many of the known strategies that might increase the survival of these cells lead to a decrease in their ability to connect to the rest of the retina. The team identified target molecules that improve the survival of the optic nerve cells and increase (not decrease) their ability to connect. The potential drug target identified is called “GCK-IV kinases,” and in the past, we showed that blocking this molecule improved the survival of both damaged cells in the retina but also cells generated in the laboratory.
During this past year, we have extended these results to investigate if blocking this molecule could improve the survival of the cells after transplantation. To date, we have obtained very promising results indicating that this strategy increases cell survival by several folds. A major barrier to optic nerve cell transplantation is a tissue called the inner limiting membrane (ILM). The ILM prevents the injected cells from moving out of the vitreous (the space inside the eye where they are injected) into the retina (where they need to integrate with other retinal cells). We have developed a surgical technique to remove part of the ILM in rodents and are currently testing whether this improves optic nerve cell transplantation. Moreover, we have developed an imaging technique to test whether the transplanted cells are making useful connections with the rest of the retina.
Finally, it is well known that optic nerve cells are not all the same and that subtypes exist. The CFC3 investigators established that certain subtypes were more resistant to glaucoma while others were more sensitive. This seemed to correlate with the expression of a protein called osteopontin (i.e., more resistant cells had higher levels). To confirm the hypothesis that osteopontin was responsible for protecting optic nerve cells, the team added osteopontin to the retina and showed that susceptible cells became resistant. Conversely, if they removed osteopontin, resistant cells became more sensitive. We also showed that osteopontin might be a potential biomarker of glaucoma.
In addition, CFC3 researchers have been working together to develop new approaches to examine how precise connections are built from the eyes to the brain, integrating imaging-based tools to understand how the connections are determined, which lays a foundation for vision restoration.
Taken together, the team has several exciting candidate targets to improve optic nerve cell survival. To translate this to the clinic, they have developed a model of glaucoma that can be used to test whether these strategies are likely to work in humans. With these new surgical techniques, imaging-based tools, and drug targets, the team will spend this next year improving optic nerve cell transplantation.
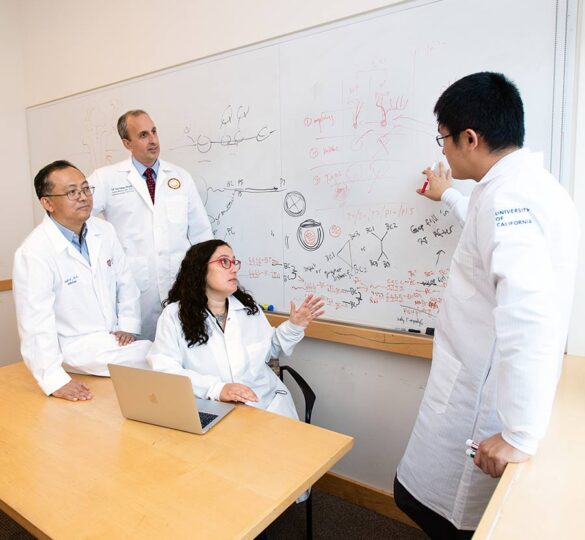
The principal investigators in the Catalyst for a Cure Vision Restoration Initiative (pictured above left to right) are Yang Hu, MD, PhD (Stanford University), Derek Welsbie, MD, PhD (UC San Diego Shiley Eye Institute), Anna La Torre, PhD (UC Davis), and Xin Duan, PhD (UC San Francisco).
This research update report was posted on March 29, 2023.